Abstract

Objective In order to understand the clinical characteristics, disease progression and survival of polycythemia vera (PV) patients, explore the risk factors affecting thrombosis in PV patients, and establish a new prognostic integral model that is consistent with the characteristics of thrombosis in PV patients in China.
Methods The clinical features, laboratory features, thrombosis, myelofibrosis transformation, leukemia transformation and survival of 975 patients with PV were studied retrospectively. By comparing the expected survival of a healthy Chinese population with age-sex matching, using the mortality rate of healthy Chinese as a reference, we calculated the standardized mortality ratio (SMR). The qualitative data were compared by the chi-square test or Fisher's test. ROC curve was used to determine the cutoff value of continuous variables, and Mann-Whitney U test and Kruskal-Wallis test were used for grouping comparison. The Kaplan-Meier method was used for survival analysis. Multivariate analysis was performed using the Cox regression model to analyze the risk factors of thrombosis and survival in patients with PV, and to establish a prognostic model for patients with PV.
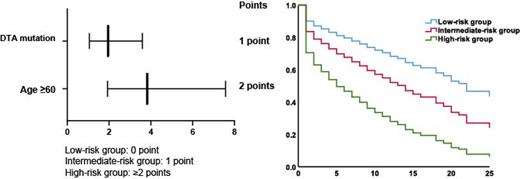
Results Results showed that among the 975 PV patients, 98.8% patients with JAK2 V617F mutation, 115 patients (11.8%) died, 202 patients (20.7%) developed secondary myelofibrosis, and 22 patients (2.3%) converted to acute myeloid leukemia. The median follow-up time of 975 patients with PV was 8(1 to 38) years in which the incidence of thrombosis was 5.4/100(95%CI[5.31/100,6.09/100]),the incidence of myelofibrosis transformation was 2.91(95%CI[1.45/100,5.15/100]), and the incidence of acute myeloid leukemia transformation was 0.28/100(95%CI[0.07/100,0.43/100]). A total of 339 patients (34.8%) had thrombosis, among which 93.2% (316/339) had arterial thrombosis and 20.1% (68/339) had venous thrombosis. Multivariate analysis shows that: Age ≥60 years old (P<0.0001, HR=3.824, 95%CI[1.930, 7.579]),DTA mutation (P=0.031, HR=1.953),95%CI[1.062,3.592 ])are risk factors for thrombosis in PV patients. According to the results of multivariate analysis, the risk model of PV thrombosis system (PTPSS) was established. In the low-risk group (0 points), the intermediate -risk group (1 points) and the high-risk group (≥2 points), the incidence of thrombosis in the high-risk group was 77.3%, 38.8% and 29.8%, respectively.The results of thrombosis survival analysis showed that: high-risk group patients (n=44;The median thrombosis-free survival was 6 years,95%CI[1.413; 10.587]), patients in the intermediate-risk group (n=304;The median thrombosis-free survival was 18 years.95%CI[10.971; 25.029]), patients in the low-risk group (n=627; The median thrombosis-free survival was 22 years.95%CI[16.797; 27.203]).
Conclusions Thrombosis is one of the most common disease progression in PV patients, and the incidence of arterial thrombosis is significantly higher than that of venous thrombosis. Even after treatment, the incidence of thrombosis is still high. PTPSS can effectively predict thrombosis in PV patients, and is a more reasonable prognostic model for guiding the prevention and treatment of PV thrombosis. We will further explore the relationship between monocytes and inflammatory factors and thrombosis in patients with PV.
No relevant conflicts of interest to declare.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal